Arthritis is a well-known and common health condition. Often thought of as an ailment that people develop as they grow older, arthritis causes painful joint age in individuals of varying health. But what many people don’t realize about arthritis is there are different types of the condition – and it can cause both crippling pain and serious health complications.
One of these types of arthritis is ankylosing spondylitis. Considered a rare variety of arthritis, ankylosing spondylitis affects more than 1 percent of the U.S. population. And that means more people are currently living with ankylosing spondylitis than multiple sclerosis, cystic fibrosis, and Lou Gehrig’s disease combined.
Fortunately, ankylosing spondylitis is a type of arthritis that can be detected early. If you know about this chronic joint condition, you may be able to catch it in its earliest stages. In order to do this, though, you need to know the facts about ankylosing spondylitis.
Ankylosing Spondylitis is a Chronic Condition
Arthritis is a chronic condition, which means it can come and go throughout a person’s lifetime. And because ankylosing spondylitis (AS) is a type of arthritis, it too is a chronic condition. Once you develop AS, you’ll likely deal with its effects for the rest of your life.
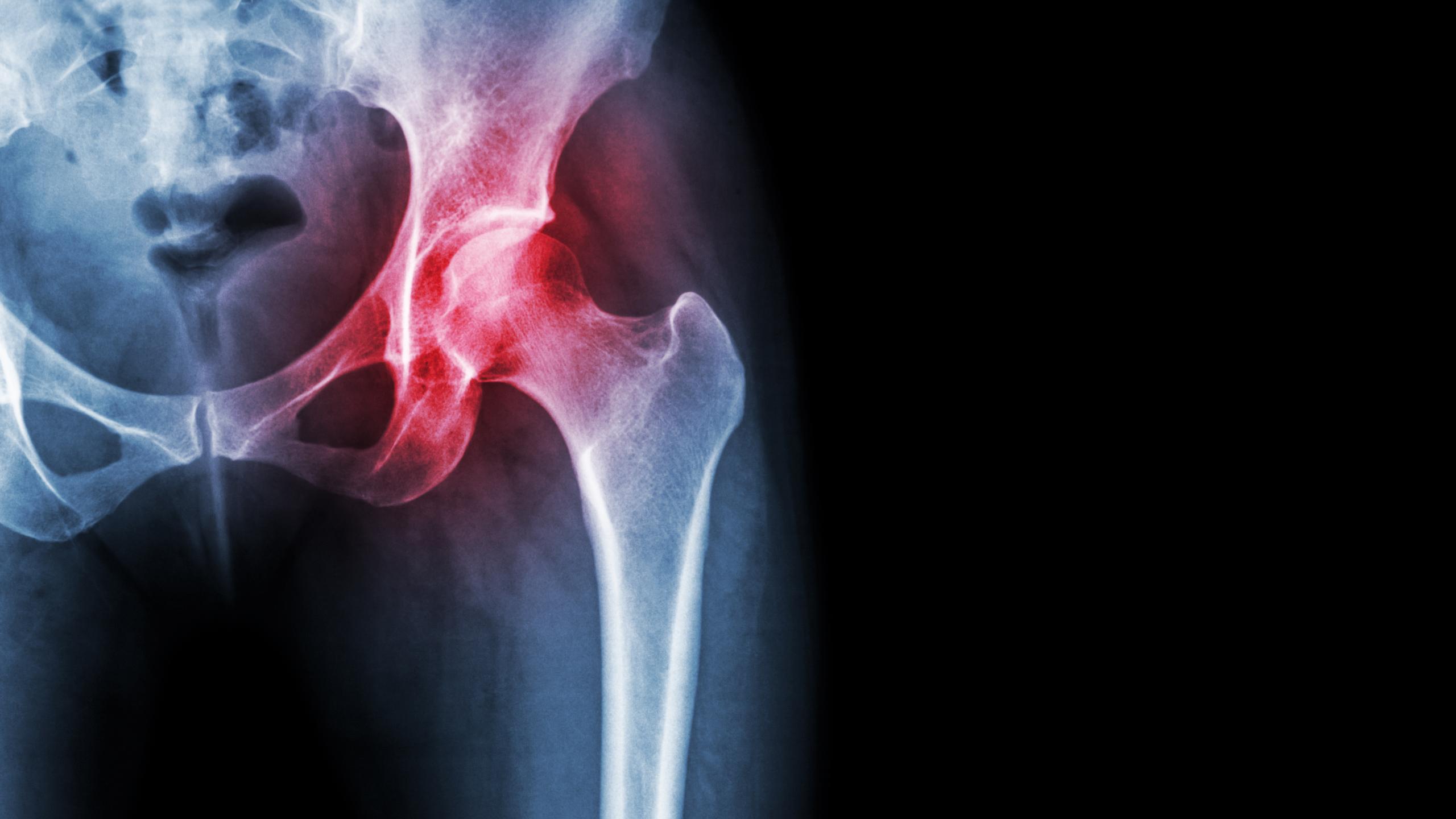
Ankylosing spondylitis is almost a more specific or localized type of arthritis. It primarily affects the joints, causing inflammation and joint damage over time. Commonly, those living with AS experience pain and stiffness in the spine. This pain often begins in the lower back, then spreads upwards to the neck and other joints.
As you grow older, AS can worsen. That’s why it’s so important to notice potential symptoms of this condition as early as possible. However, if left untreated, it can cause growing pain and increasing health problems. For example, ankylosing spondylitis can cause the spine’s vertebrae to fuse together, which leads to limited movement and flexibility.
Currently, there is no cure for AS. Those living with this condition must try to slow the disease’s progression and alleviate its symptoms with certain management and treatment options.
Anyone Can Develop Ankylosing Spondylitis
Just like arthritis, anyone can develop ankylosing spondylitis. However, researchers are still unclear as to what causes or triggers AS.
AS may be a genetic condition. Researchers have discovered that individuals who are diagnosed with AS also have gene HLA-B27, which is connected to the body’s immune system. When this specific gene is present, the immune system attacks bacteria, which then appears to trigger AS symptoms.
Based on this information, anyone who has the HLA-B27 gene may be at an increased risk for developing ankylosing spondylitis. To know if this is the case, it’s a good idea to talk with your doctor.
Additionally, men may be at a higher risk of developing AS than women. It’s been found that men tend to develop AS more frequently than women, and it’s a condition that typically appears in men at a younger age.
Symptoms of Ankylosing Spondylitis
Ankylosing spondylitis is a condition that usually begins exhibiting symptoms early on. When the condition first begins, it brings symptoms like pain and stiffness in the lower back and hips.
You might not immediately connect the symptoms you experience with AS. The very first symptoms can be subtle – for example, feeling stiffness or pain when you wake up in the morning or after sitting down for long periods of time.
Other symptoms can also appear early on. These may include neck pain and fatigue. Symptoms, particularly aches and pain, may worsen. They might also disappear or occur infrequently.
But as AS progresses, it starts to present its symptoms more consistently. Pain becomes more frequent, and you’ll likely experience both pain and stiffness in:
- The base of your spine.
- Your lower back.
- Specific lower back vertebrae.
- Places where tendons and ligaments attach to bones.
- Hip joints.
- Shoulder joints.
If you’re concerned that you might be experiencing symptoms of AS, make sure to speak with your doctor. A doctor is the only person who’ll be able to give you a firm answer and a diagnosis. Set up an appointment to discuss your symptoms so you can find out if AS is truly the problem.
How Ankylosing Spondylitis is Treated and Managed
Once you’ve been diagnosed with ankylosing spondylitis, it’s important to discuss your management and treatment options with your doctor. Managing AS is key in reducing your pain and preventing complications, such as joint damage or other health conditions.
Because there is no treatment for AS, you may need to rely on a number of different management strategies to keep the condition under control.
The following are commonly prescribed treatments for individuals with AS:
- Regular exercise: Getting regular exercise can help with flexibility, pain, and posture.
- Medication: Over-the-counter medications, as well as some prescription medications, may alleviate some of the inflammation and pain caused by AS.
As your ankylosing spondylitis changes over time, you may experience different symptoms and require different management or treatment options. Remember, AS can progress – and that means it can worsen over years. As this happens, you may see your symptoms and your health also worsen.
When complications occur, they often include the following:
- Pain and inflammation in the spine, hips, and pelvis.
- Eye problems that cause blurry vision or sensitivity.
- Heart problems, like an enlarged aorta or changes in shape of the aortic valve.
- Certain types of cancer.
Ultimately, if you’re worried about ankylosing spondylitis, your best course of action is information. Knowing the facts about AS can help you recognize its signs, symptoms, and potential complications. And that can give you the opportunity to catch AS early.
If you begin experiencing any of the symptoms of AS, find a doctor who can test you for the condition. It’s important to either confirm a diagnosis or rule out AS. From there, you’ll be able to take the right steps for your health.